Scleroderma is a rare autoimmune illness in which the immune system attacks the body. In this instance, an overabundance of collagen is produced because the immune system misidentifies normally healthy tissues as an infection or foreign substance. Extra collagen is subsequently deposited in the skin and organs, causing thickening and hardness that resembles a scar.
While the skin is the most usually afflicted organ, this disease can also affect the muscles, digestive system, lungs, kidneys, blood vessels, and heart. The exact cause of the disease is uncertain. Also, there is no cure for it. However, there are treatments to alleviate the symptoms.
In this article, we are going to discuss more regarding scleroderma, from its symptoms to its treatment. Keep on reading!
What is Scleroderma?
Scleroderma is an autoimmune connective tissue and rheumatic disease that causes inflammation in the skin and other parts of the body. When the immune system fools tissues into believing they are harmed, it causes inflammation and makes the body produce excessive collagen, resulting in scleroderma. Excess collagen in your skin and other tissues generates patches of tight, hard skin.
Scleroderma commonly strikes adults between the ages of 30 and 50, and it affects more women than men. This disease is neither infectious nor contagious, thus you cannot catch it from someone else. Although there is no cure, treatment can reduce your symptoms and make you feel better.
What are the Types of Scleroderma?
Scleroderma is characterized by the development of circumscribed or hard, smooth, ivory-colored areas that are immovable and gives the impression of hidebound skin, and it can occur in both localized and systemic forms.
- Localized scleroderma only affects the skin and the structures directly under the skin. There are two main forms of localized scleroderma which are:
- Morphea: Patches of hard skin form and can last for years.
- Linear: Scleroderma thickening occurs in a line, usually extending down an arm or leg but sometimes running down the forehead and face.
- Systemic scleroderma affects the circulation of the blood and internal organs, such as the heart, lungs, and kidneys. This form has two main types which are:
- Limited (CREST Syndrome): Affects the skin of the hands, feet, face, lower arms, and legs. It might also cause issues with the blood vessels, lungs, or digestive system.
- Diffuse: Affects the area from the hands to above the wrists, and also internal organs. It causes weakness, weariness, breathing and swallowing difficulties, and unintended weight loss.
What are the Symptoms of Scleroderma?
Scleroderma might result in a wide range of different symptoms and complications. For some, it is a lifelong discomfort; for others, it is a condition that rapidly progresses and may lead to death. Potential signs and symptoms include:
- Hard skin
- Pain and stiffness in the joints
- Digestive problems
- Difficulty swallowing
- Puffy hands and feet
- Muscle weakness
- Unintended weight loss
- Fatigue
- Red spots on the skin
- Ulcerations on the fingertips and toes
- Persistent cough
- Shortness of breath
- Heartburn
- Diarrhea
- Hair loss
What Causes Scleroderma?
Although the exact cause of scleroderma is uncertain, researchers believe that a variety of factors may be involved:
- Genetics: Genes can enhance the likelihood of some people developing scleroderma and play a role in defining the type of scleroderma they have. Like several hereditary diseases, this one cannot be inherited and is not transferred from parent to kid. However, compared to the general population, first-degree relatives of scleroderma patients have a greater chance of contracting the disease.
- Immune system changes: Abnormal immunological or inflammatory activity in your body causes cell alterations that lead to excessive collagen formation.
- Hormones: In most cases, scleroderma affects women more frequently than it does men. Researchers suspect that hormonal variations between men and women may contribute to the condition.
- Environment: Scleroderma may be brought on by exposure to certain external conditions, such as chemicals or viruses.
How is Scleroderma Diagnosed?
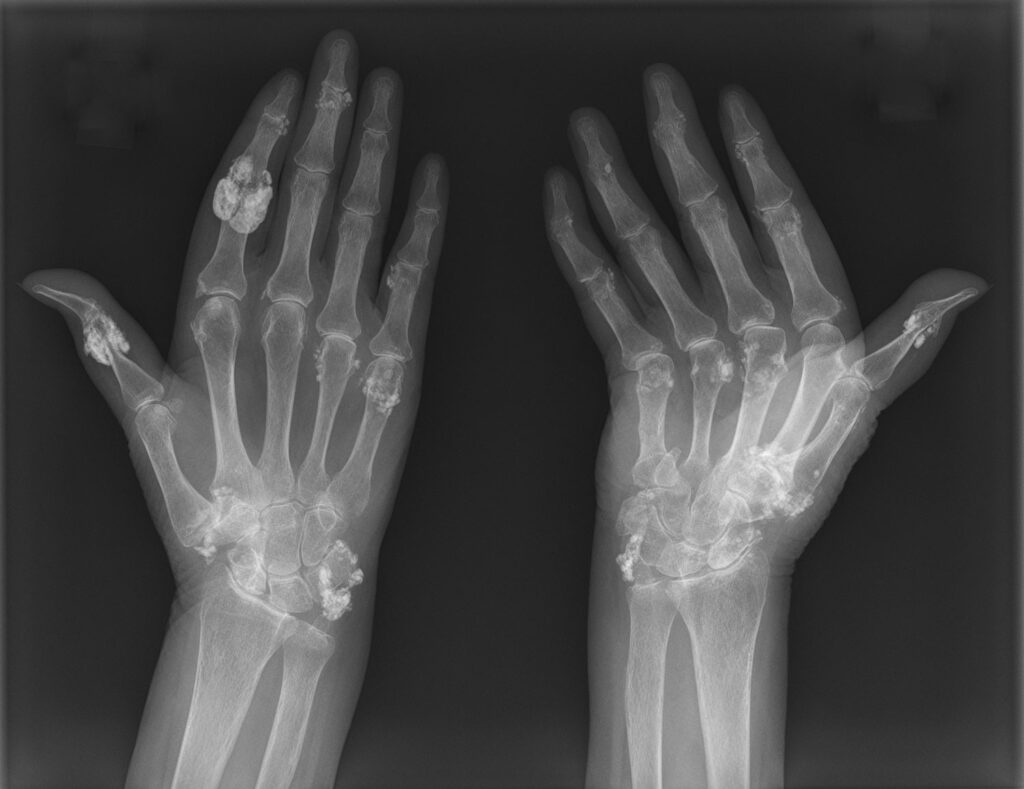
Scleroderma can be challenging to diagnose since it develops in different forms and progresses gradually. First things first, your doctor will be on the lookout for all of the symptoms, particularly for any thickening or hardness of the skin around the fingers and toes. If scleroderma is suspected, testing will be prescribed to confirm the diagnosis and identify the disease’s severity. These tests might consist of:
- Blood tests: About 95% of scleroderma patients have elevated levels of immunological factors called antinuclear antibodies. Although these antibodies can be seen in other autoimmune disorders such as lupus, testing for them in suspected scleroderma patients can aid in an accurate diagnosis.
- Pulmonary function tests: These examinations are performed to evaluate how effectively the lungs are working. If scleroderma is suspected or confirmed, it is critical to determine whether or not it has migrated to the lungs, where scar tissue development might occur. Lungs condition can be examined using an X-ray or a CT scan.
- Gastrointestinal tests: Scleroderma can damage both the esophageal muscles and the intestinal walls. This can induce heartburn and difficulties swallowing, as well as affect nutrient absorption and food flow through the gut. Endoscopy is occasionally performed to observe the esophagus and intestines.
- Electrocardiogram: Scleroderma can result in cardiac tissue scarring, which can trigger congestive heart failure and irregular heart electrical activity. This test determines whether the disease has impacted the heart.
- Kidney function: Scleroderma can impact the kidneys, which can lead to protein leakage into the urine and a rise in blood pressure. In its most severe condition, there may be a sudden rise in blood pressure that leads to kidney failure.
How to Treat Scleroderma?
Scleroderma has no known cure. However, there are treatments that can help reduce symptoms and organ damage. Localized scleroderma is typically treated with topical (applied to the skin) medications like moisturizers or corticosteroid creams. Whereas systemic scleroderma can be treated with medications that enhance blood flow, stimulate esophageal and bowel function, keep the kidneys functioning, and lower high blood pressure.
Because there are no effective and specific treatments, researchers wanted to evaluate the response of hyaluronic acid filler injections combined with platelet-rich plasma. Recent research suggests that injections of hyaluronic acid (HA), an anionic, non-sulfated glycosaminoglycan found in connective, epithelial, and neural tissues, might be used to cure skin fibrosis.
Platelet-rich plasma (PRP) is a plasma fraction with a concentration above that of peripheral blood and the capacity to release a variety of growth factors that promote wound healing, Given that it has the ability to bind water, this treatment has the potential to fill in the gaps, soften, and moisturize the skin. Furthermore, studies have shown that it stimulates the formation of type I collagen in the dermis, which may help to explain its long-lasting effects.
According to the study, people with scleroderma can benefit locally from platelet-rich plasma and hyaluronic acid filler injections as a treatment option. These growth factors, in particular, and their roles in cell proliferation, angiogenesis, and inflammation reduction, explain why PRP is being used in this novel treatment. PRP treatment has significantly improved the patient’s quality of life. As a matter of fact, it has ensured a good outcome from an aesthetic and functional perspective, as seen both visually and from an instrument perspective.