Rheumatoid arthritis is a chronic disease that affects the joints and results in pain, swelling, and stiffness. Typically, the condition affects the hands, feet, and wrists. There may be periods when symptoms worsen, which are referred to as flare-ups or flares. A flare might be difficult to anticipate, but treatment can reduce the number of flares and minimize long-term joint damage. Some patients with rheumatoid arthritis may have issues with other body parts or more general symptoms like fatigue and weight loss. There is no cure for rheumatoid arthritis, but treatments can improve symptoms and slow the progress of the disease. One of the best treatments for rheumatoid arthritis patients by using platelet-rich plasma (PRP) with disease-modifying antirheumatic medications (DMARDs) as its basis.
What is Rheumatoid Arthritis?
Rheumatoid arthritis, often known as RA, is an autoimmune and inflammatory condition in which your immune system unintentionally attacks healthy cells in your body, leading to inflammation (painful swelling) in the areas of your body affected.
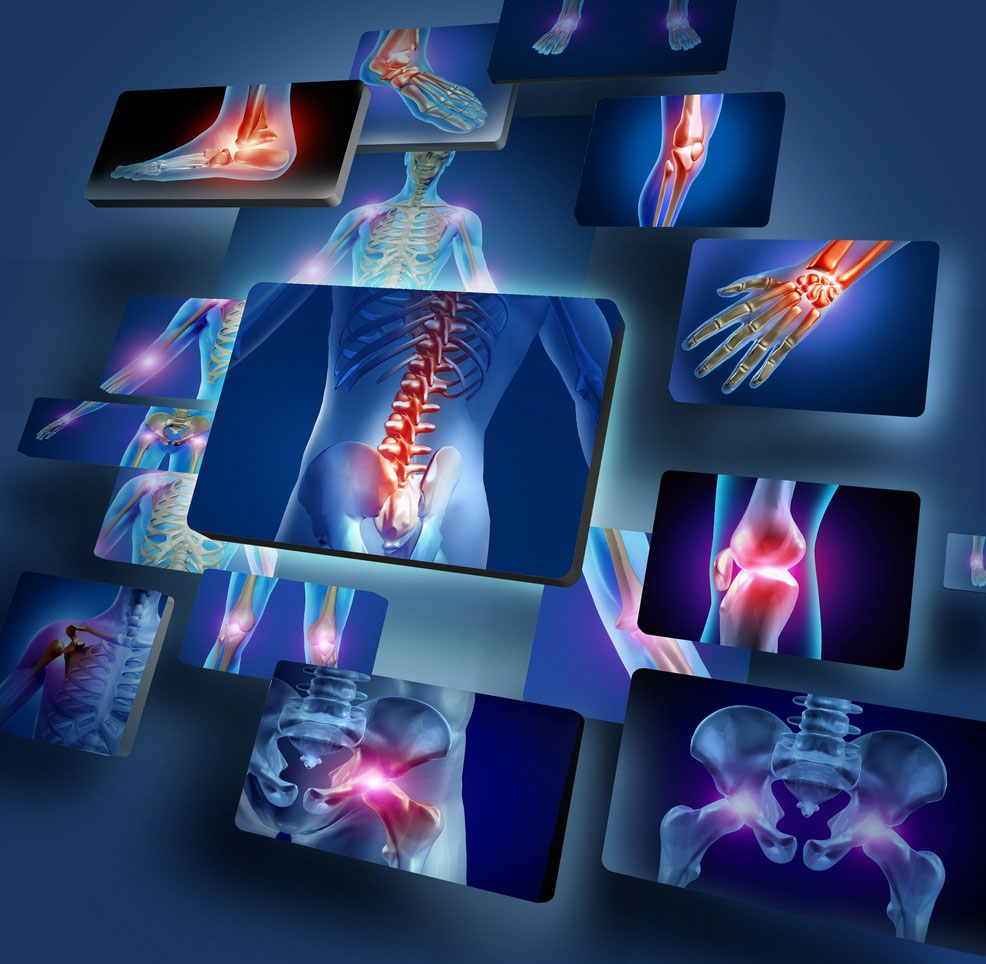
Rheumatoid arthritis (RA) causes joint inflammation and pain. This occurs when the synovium, the lining of the joints, is attacked by an immune system that isn’t functioning correctly. The condition frequently affects the hands, knees, or ankles, and typically the same joint on both sides of the body, such as both hands or both knees. When RA affects a joint, the joint’s lining becomes inflamed, harming the joint tissue. This tissue damage can result in long-term pain, unsteadiness (loss of balance), and deformity (misshapenness). RA can also affect other parts of the body, such as the eyes, heart, circulatory system, or lungs.
What are the Symptoms of Rheumatoid Arthritis?
Rheumatoid arthritis affects people differently. Some people develop joint symptoms over several years. In some patients, rheumatoid arthritis symptoms worsen quickly. Many patients experience flare-ups of symptoms followed by periods of time with no symptoms (remission).
The following symptoms of RA include:
- Pain and stiffness in more than one joint
- Tenderness and swelling of joints
- Weight loss
- Fatigue
- Weakness
- Fever
What Causes Rheumatoid Arthritis?
The exact cause of rheumatoid arthritis is unknown. Researchers believe it is caused by a combination of factors, such as genetics, hormones, and environmental factors.
Normally, the immune system battles foreign invaders such as germs and viruses. In autoimmune diseases like RA, the immune system misidentifies the body’s cells as foreign invaders and releases inflammatory substances that attack those cells. Moving the joint may be challenging due to the thickening of the inflammatory synovium, which also causes the joint to look red, swollen, and also painful. This condition could also be triggered by smoking, an infection, or stress.
How is Rheumatoid Arthritis Diagnosed?
RA is diagnosed by examining symptoms by reviewing medical history, performing a physical examination, ordering X-rays, and lab testing. Early RA diagnosis is preferred, ideally within six months of the beginning of symptoms, to allow patients to start treatment and delay or stop the disease’s progression. Treatments that suppress or manage inflammation in particular can help decrease inflammation and lessen the negative consequences of RA.
- Medical history: The doctor will inquire about joint symptoms (pain, soreness, stiffness, trouble moving), when they started, if they come and go, how severe they are, what actions make them worse or better, and whether any family members have RA or another autoimmune disease.
- Physical examination: The doctor will check for joint soreness, swelling, warmth, and painful or limited movement bumps beneath the skin, as well as a low-grade fever.
- Blood tests: The blood tests are done to look for inflammation and blood proteins (antibodies) that are linked to RA. Commonly performed blood tests are erythrocyte sedimentation rate (ESR), c-reactive protein (CRP), rheumatoid factor (RF), and cyclic citrullinated peptides (CCP) (proteins).
- Imaging tests: RA can cause the ends of bones within a joint to deteriorate (erosions). Erosion detection can be done using an X-ray, ultrasound, or MRI scan. However, if they don’t appear on the initial tests, it may indicate that RA is still in the early stages and hasn’t damaged bone yet. Imaging data can also indicate how well a treatment is working.
How to Treat Rheumatoid Arthritis?
Patients with RA should begin their treatment with disease-modifying antirheumatic medications (DMARDs). These medications not only ease the signs and symptoms, but they help stop the joint damage from getting worse. Doctors frequently prescribe DMARDs together with nonsteroidal anti-inflammatory medications, NSAIDs, and/or low-dose corticosteroids to reduce swelling and discomfort.
DMARDs have significantly reduced pain, swelling, and quality of life in almost all RA patients. DMARDs include methotrexate (Rheumatrex, Trexall, Otrexup, Rasuvo), leflunomide (Arava), hydroxychloroquine (Plaquenil), and sulfasalazine (Azulfidine). Cyclosporine and Azathioprine may be taken on occasionally, but not as regularly as other medications that are more effective.
With DMARDS as the basis, platelet-rich plasma (PRP) has been the focus of study in numerous fields during the past ten years. Researchers are experimenting with PRP for RA due to its potential to halt and reverse inflammation.
Researchers suggest a valuable role of PRP in patients with rheumatoid arthritis, specifically patients who fail therapy with one or more of the other medications. PRP may be an effective and safe treatment for RA patients who are failing to react to conventional treatments as their condition worsens. Intra-articular PRP may be easier to implement in RA patients because it is delivered in outpatient settings and does not necessitate hospitalization. PRP could become a surgical alternative for RA patients. However, PRP preparations must be managed carefully to prevent any unintentional infection transmission.
The treatment area is injected with growth factors, fibrin, and other healing agents thanks to the PRP, which has 5–10 times the typical amount of platelets. Growth factors encourage your body to make more fibrin and endothelial cells, which lessen joint inflammation. Additionally, the PRP encourages your body to grow more healthy blood vessels, which improves blood circulation. Over a series of treatments, your body starts to repair injured cartilage. The PRP stimulates your body’s natural healing processes, which were decelerated by your disease. The PRP injections help your body in getting advantages.